In recent years, the discourse surrounding alcohol consumption and its implications for health has intensified, revealing layers of complexity that warrant careful consideration. For individuals who have faced the harrowing journey of breast cancer, the relationship between alcohol and the risk of recurrence has emerged as a particularly poignant topic. Research indicates that even a handful of glasses of alcohol per week can significantly elevate the risk of breast cancer returning, igniting a shift in the way survivors and healthcare professionals alike perceive this common social lubricant.
The crux of the matter lies in the biochemical pathways influenced by alcoholic beverages. Ethanol, the intoxicating component of alcohol, undergoes metabolism in the liver, leading to the production of acetaldehyde—an agent recognized as a probable human carcinogen. This transformation sparks a cascade of biological reactions that may inadvertently promote the proliferation of malignant cells and undermine the body’s ability to combat cancer recurrence.
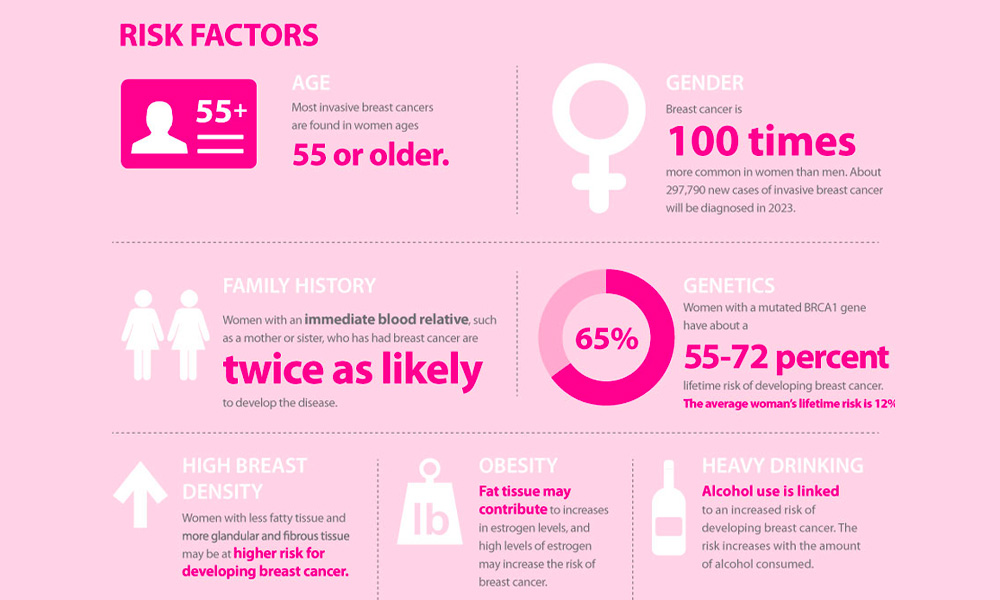
Moreover, alcohol may interfere with hormonal balance, particularly estrogen levels in women. As breast cancer is often hormone receptor-positive, fluctuations in estrogen induced by alcohol consumption could potentiate the reemergence of tumors. This connection has prompted oncologists to urge a reevaluation of drinking habits among breast cancer survivors, advocating for heightened awareness of how seemingly innocuous decisions can carry significant ramifications for long-term health.
Amidst this backdrop of concern, the nuance of moderation comes into play. While some studies suggest that the risks escalate with increased alcohol intake, the definition of moderation might vary greatly between individuals. What one person perceives as a reasonable drink or two per week may stand in stark contrast to another’s experience. Thus, the call for personalized guidelines becomes paramount, necessitating dialogue between patients and their healthcare providers to navigate these treacherous waters.
This burgeoning understanding urges a cultural shift away from the normalization of alcohol consumption. Social settings often imbue drinking with a sense of conviviality and relaxation, yet for breast cancer survivors, this social contract can come at a cost. The benefits of recalibrating social engagements to include alternatives to alcohol transcend mere personal health—they encapsulate a broader movement toward wellness-centric lifestyles.
In conclusion, the interaction between alcohol consumption and the risk of breast cancer recurrence serves as a critical reminder of the multifaceted nature of health. As research continues to unfold, it becomes increasingly clear that even a few glasses of alcohol per week can bear consequences that extend beyond immediate enjoyment. This revelation beckons a moment of contemplation, urging survivors to reconsider the implications of their choices in the broader context of their health journeys.