When it comes to managing diabetes and weight, GLP-1 (glucagon-like peptide-1) medications have garnered increasing attention for their efficacy. Particularly, medications like Ozempic have emerged as game-changers in the health landscape. But for individuals without a gallbladder, the question arises: Can I take GLP-1 without a gallbladder? This inquiry reflects a broader fascination with how our bodies interact with medications and the implications of anatomical differences on pharmacological efficacy.
The role of the gallbladder is often underestimated. This small organ, situated beneath the liver, is primarily responsible for storing bile, a digestive fluid produced by the liver that aids in fat digestion. The absence of a gallbladder can lead to significant changes in how fats are processed and absorbed in the body. It’s crucial to consider how such a fundamental alteration may affect the use of GLP-1 medications.
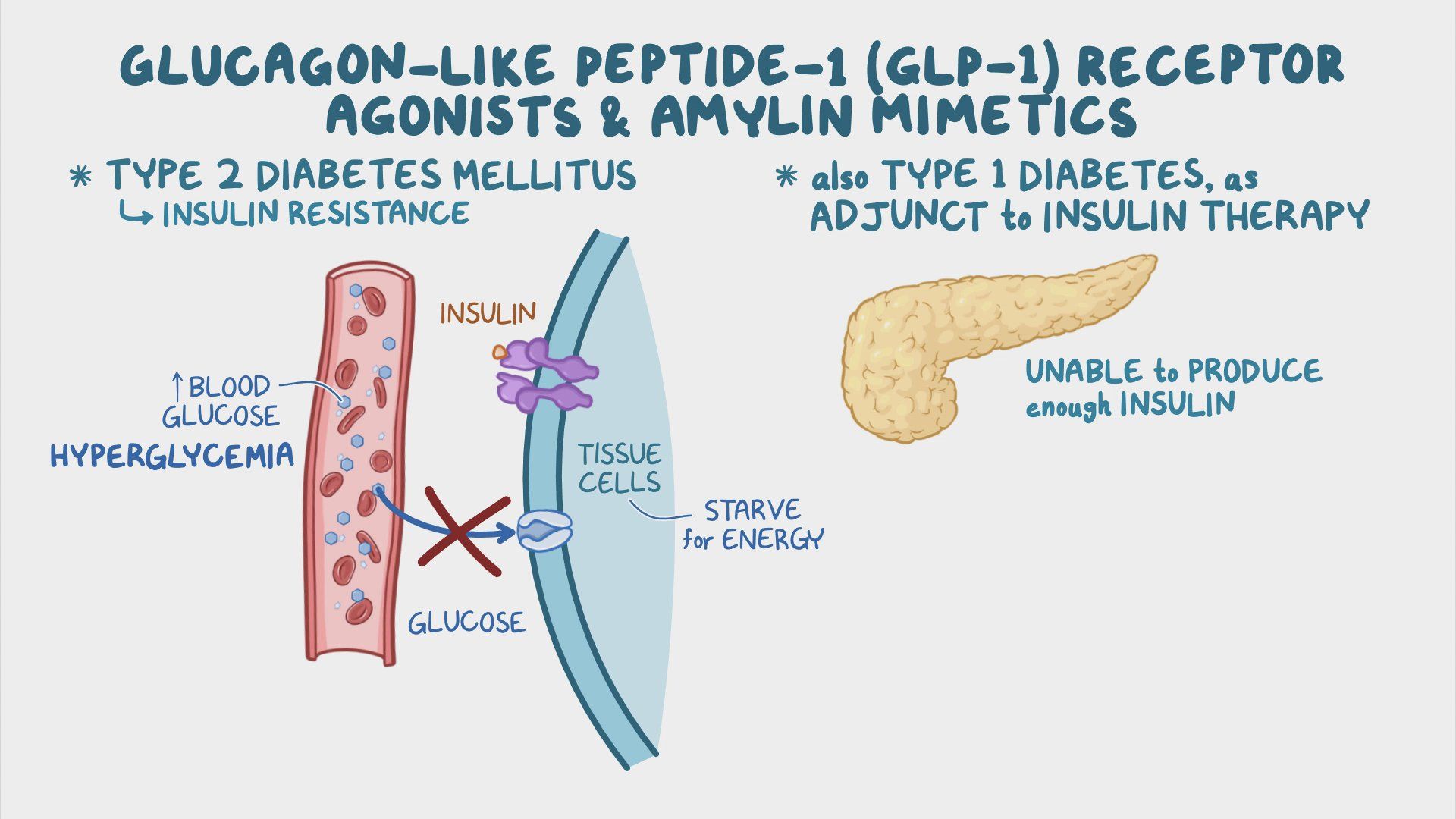
Firstly, understanding GLP-1 medications is essential. These drugs, primarily indicated for type 2 diabetes, work by mimicking the action of the naturally occurring hormone glucagon-like peptide-1 which plays a pivotal role in glucose metabolism. They stimulate insulin secretion, inhibit glucagon release, slow gastric emptying, and promote satiety. This combination of actions not only helps in regulating blood sugar levels but also facilitates weight loss—a noteworthy advantage for many patients.
For individuals who have undergone cholecystectomy, or gallbladder removal, the digestibility of food, particularly fats, is altered. Without the gallbladder’s concentrated bile, some patients may experience difficulty digesting fatty meals. This can manifest as gastrointestinal discomfort, bloating, or diarrhea. Considering these nuances is essential when introducing a GLP-1 medication to those without a gallbladder.
One significant consideration is the absorption of the medication. While GLP-1 medications are administered via subcutaneous injection, their systemic absorption can potentially be influenced by gastrointestinal transit times. Individuals without a gallbladder may experience rapid gastric emptying (also known as dumping syndrome), which could alter the pharmacokinetics of the medication. Clinically, this suggests a need for close monitoring when initiating GLP-1 therapy in patients with this anatomical variation.
Moreover, the interaction between GLP-1 medications and dietary habits bears examination. Since these medications enhance feelings of fullness, adherence to a diet low in fast-acting carbohydrates and rich in nutrients becomes paramount. For those without a gallbladder, it’s advisable to consume smaller, more frequent meals and to be vigilant regarding fat intake. Balancing the advantageous effects of GLP-1 medications with these dietary adjustments can be an interesting challenge that compounds the treatment journey.
Another layer of complexity lies in the medication’s side effects. Gastrointestinal issues are common with GLP-1 medications, including nausea, vomiting, and diarrhea. While individuals with a gallbladder may experience these side effects, those without one could potentially encounter exacerbated symptoms. Therefore, healthcare providers must adopt a tailored approach to dosing and management, ensuring that patients are adequately informed about what to expect.
Furthermore, individual responses to medications can vary widely based on an array of factors, including lifestyle, concurrent health conditions, and body composition. For individuals without a gallbladder, this leads to the importance of personalized medical advice. It’s not just about whether they can take GLP-1 medications, but also how they can maximize its efficacy while minimizing side effects. This emphasizes the notion that there’s often no one-size-fits-all answer in medicine.
Considering alternative GLP-1 strategies may also be beneficial. In some cases, oral versions of GLP-1 medications are available. The decision to transition from injectables to oral formulations should consider digestive capabilities. Reviewing and adjusting medication regimens to align with one’s digestive health can lead to more fruitful outcomes in both weight management and blood sugar control.
As we dissect the interplay between anatomy and pharmacology, another poignant point emerges: the sense of empowerment that comes from understanding one’s body and health. Patients can take an active role in their health care. They should engage with healthcare providers regarding their anatomy, medication plans, and any concerns related to dietary adjustments. The journey through chronic illness or metabolic disorders can be daunting; however, knowledge can help alleviate fears and foster confidence.
In conclusion, while taking GLP-1 medications without a gallbladder is feasible, it requires a nuanced approach that considers digestive changes, personalized medicine, and the importance of patient engagement. The fascination lies not just in the medication’s ability to manage diabetes and weight loss, but in the intricate relationship between human anatomy, pharmacology, and individual wellness. Such insights not only enhance our understanding of treatment options but also illuminate the significance of tailoring health care to accommodate unique physiological contexts.