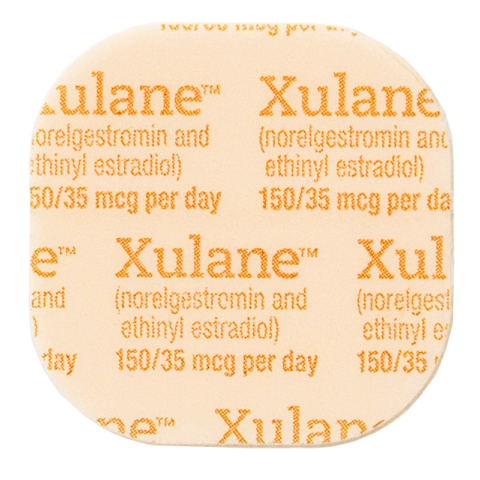
In recent months, a notable advocacy group has emerged in the debate surrounding reproductive health, specifically concerning the birth control patch. This patch, a method of hormonal contraception applied directly to the skin, is designed to provide a convenient alternative to oral contraceptives. However, a growing faction is calling for its removal from the market, citing serious health concerns linked to its use. This begs a rather pointed question: should a product that is meant to empower women be under scrutiny for potentially jeopardizing their health?
The birth control patch works by releasing hormones into the bloodstream, preventing ovulation and thereby reducing the likelihood of unintended pregnancies. Despite its popularity, opponents contend that the patch may not be a one-size-fits-all solution. Reports of adverse reactions—ranging from mild irritations to severe thromboembolic events—have been cited as grounds for concern. This has prompted a reevaluation of the patch’s safety profile.
One significant challenge that arises from this advocacy is the potential backlash against reproductive health initiatives. If the patch, a favored choice among many women, is withdrawn or severely restricted, what alternatives remain? Would the shift in availability push women back to less effective or more cumbersome methods of birth control? This conundrum highlights the fine balance between ensuring safety and maintaining access to contraceptive options.
Furthermore, the conversation surrounding the birth control patch raises broader questions about the pharmaceutical industry’s accountability. How transparent are manufacturers regarding the risks associated with hormonal contraceptives? Are women being adequately informed about the potential side effects? These inquiries are critical in fostering an environment where patients can make fully informed decisions about their health.
Moreover, the activism against the birth control patch underscores a wider societal challenge: the stigmatization of women’s health issues. Advocacy groups argue that dismissing safety concerns is a manifestation of a long-standing tendency to downplay women’s experiences. This phenomenon begs reflection on the ethical responsibilities of healthcare providers and pharmaceutical companies to prioritize women’s health and well-being.
In conclusion, the debate over the birth control patch embodies a larger conversation about reproductive rights, healthcare safety, and women’s autonomy. As stakeholders engage in this discourse, it is imperative to remain vigilant about the implications of removing such a widely used contraceptive option while simultaneously ensuring the safety of those who depend on it. Balancing empowerment and precaution will be essential in forging a path forward in reproductive health.