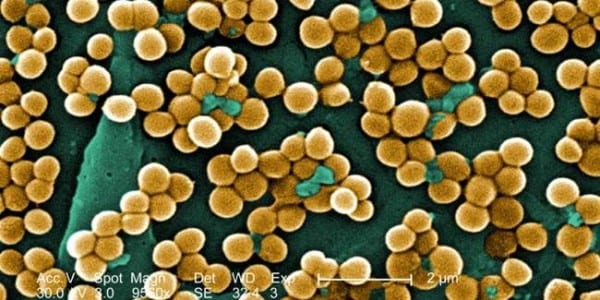
Imagine a city besieged by an unseen enemy, stealthily infiltrating the very fabric of its infrastructure. This metaphor serves as a fitting backdrop to understand the escalating threat posed by methicillin-resistant Staphylococcus aureus (MRSA), a formidable superbug that has turned hospitals and healthcare facilities into breeding grounds for infection. In the quest to reclaim safety within these walls, universal testing emerges as a beacon of hope, a proactive approach promising to stem the tide of this insidious adversary.
At its core, universal testing for MRSA is akin to installing a state-of-the-art alarm system in a house beset by intruders. Rather than waiting for symptoms to manifest or outbreaks to occur, healthcare institutions adopting this strategy opt for preemptive action. Every patient is screened upon admission, regardless of their infection history or presenting symptoms. This paradigm shift in approach amplifies the effectiveness of infection control by facilitating early identification and isolation of carriers.
The ramifications of universal testing are profound, akin to a single drop of ink dispersing in water. Initially, testing reveals the latent reservoirs of MRSA lurking within patient populations—individuals who may appear healthy yet harbor the bacteria. By identifying these hidden carriers, healthcare providers can implement targeted decolonization strategies. The result is a significant reduction in infection rates, effectively severing the chain of transmission that perpetuates MRSA outbreaks.
Moreover, universal testing fosters a culture of vigilance and accountability among healthcare workers. It empowers them with knowledge and tools to combat infections, reinforcing the importance of adherence to sanitary protocols. When each member of a healthcare team becomes a sentinel against MRSA, the collective efficacy of their efforts increases exponentially, creating a fortress of defense that can lead to eradication of this persistent pathogen.
However, the implementation of universal testing does not come without challenges. Logistics, costs, and the potential for false positives are concerns that must be addressed. Yet, much like a finely tuned machine, when integrated with existing infection control measures, the benefits far outweigh the pitfalls. Successful case studies from various institutions illustrate that hospitals embracing universal testing experience decreased rates of surgical site infections, a testament to the methodology’s potency.
In conclusion, the narrative surrounding MRSA is one of urgency and innovation. Universal testing represents an evolution in our battle against superbugs, transforming the approach to infection control from reactive to proactive. It is a clarion call for healthcare systems to fortify their defenses, safeguarding patients and preserving the sanctity of healing environments. In this ongoing odyssey against microbial adversaries, universal testing stands as both a strategy and a symbol of our commitment to public health, striving towards the goal of a healthier tomorrow.