In the realm of women’s health, the interplay between hormonal therapy and the accuracy of mammographic screenings has garnered increased scrutiny. For women utilizing estrogen and progestin, particularly those undergoing hormone replacement therapy (HRT) during menopause or for other medical indications, the implications can be profound. Recent studies have illuminated a critical correlation: these hormones may contribute to a higher incidence of false-negative mammograms.
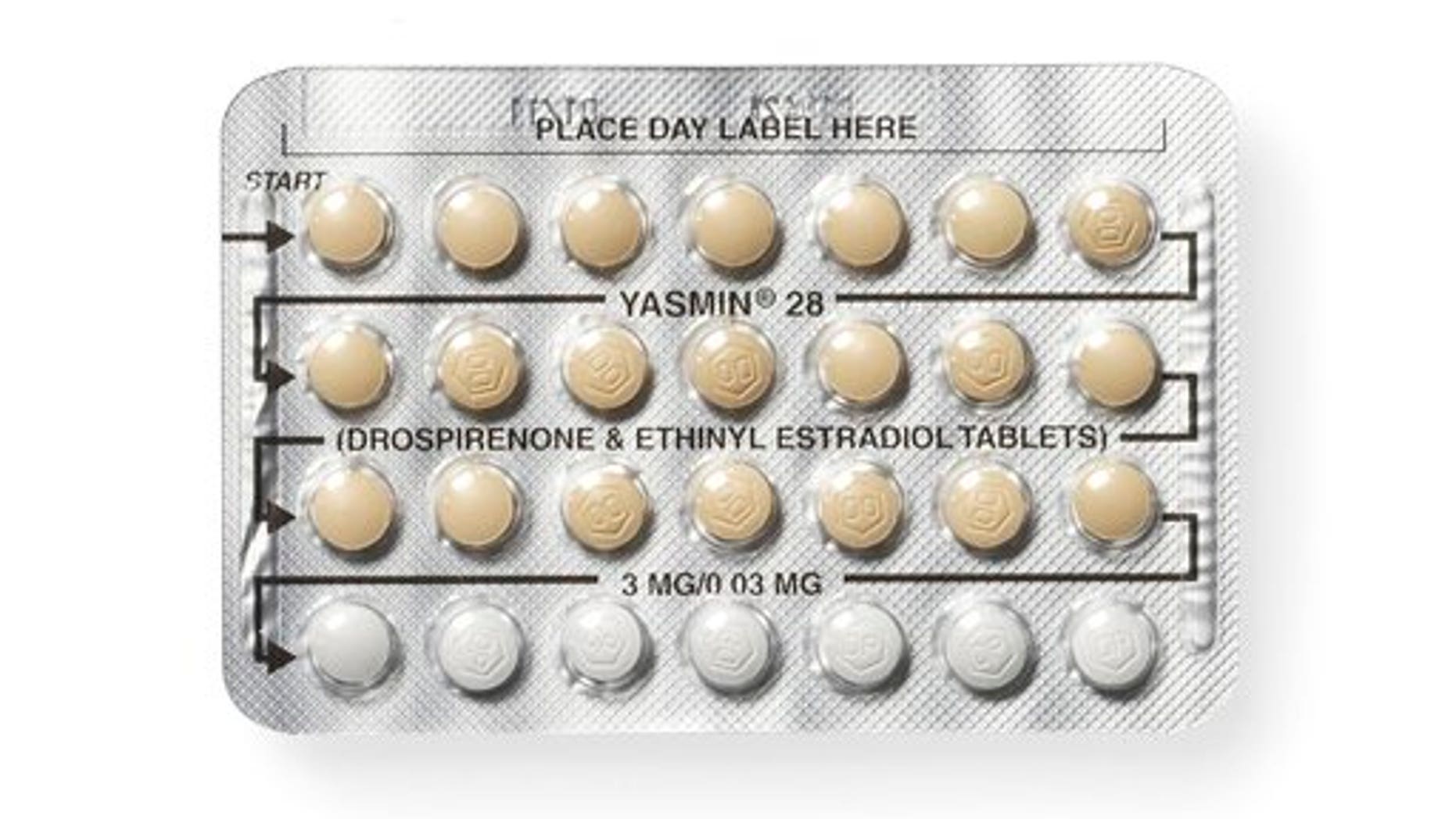
To comprehensively understand this phenomenon, it is pivotal to grasp the role of estrogen and progestin in the body. Estrogen is integral in regulating numerous physiological processes, including the menstrual cycle and reproductive system. Progestin, often administered in conjunction with estrogen, helps to mitigate the risk of endometrial hyperplasia in women with intact uteri. While these hormones offer significant benefits, their influence on breast tissue density is noteworthy.
One of the critical concerns surrounding mammograms is the impact of breast density. Mammograms can be less effective for women with denser breast tissue, which may obscure the detection of tumors. The administration of estrogen can increase breast density, thus rendering mammograms less reliable. This predicament is exacerbated in women taking both hormones, as the compounded effects can mislead radiologists, resulting in diagnostic errors.
Moreover, the potential for faulty mammograms carries an inherent risk for late-stage breast cancer diagnosis. When tumors are not identified during routine screenings, the cancer can progress undetected, leading to poorer prognoses. Women engaged in HRT must be acutely aware of their increased risk; proactive discussions with healthcare providers about personalized screening strategies are essential.
It is imperative for healthcare professionals to maintain an astute awareness of these complications. They should actively encourage patients on hormonal therapy to undergo supplementary screening modalities, such as breast ultrasounds or MRIs, especially if they present with dense breast tissue. These adjunctive imaging techniques can enhance the probability of early cancer detection and mitigate the risk of oversight associated with traditional mammography.
In conclusion, while estrogen and progestin play essential roles in women’s health, their effects on mammographic accuracy cannot be overlooked. A multifaceted approach to breast health is paramount, underpinning the necessity for tailored screening practices for women on hormonal therapy. By fostering informed dialogues between patients and healthcare providers, the medical community can enhance the efficacy of breast cancer screening and ultimately save lives.